Online Yoga Therapy Course: Healing Through Ancient Practice
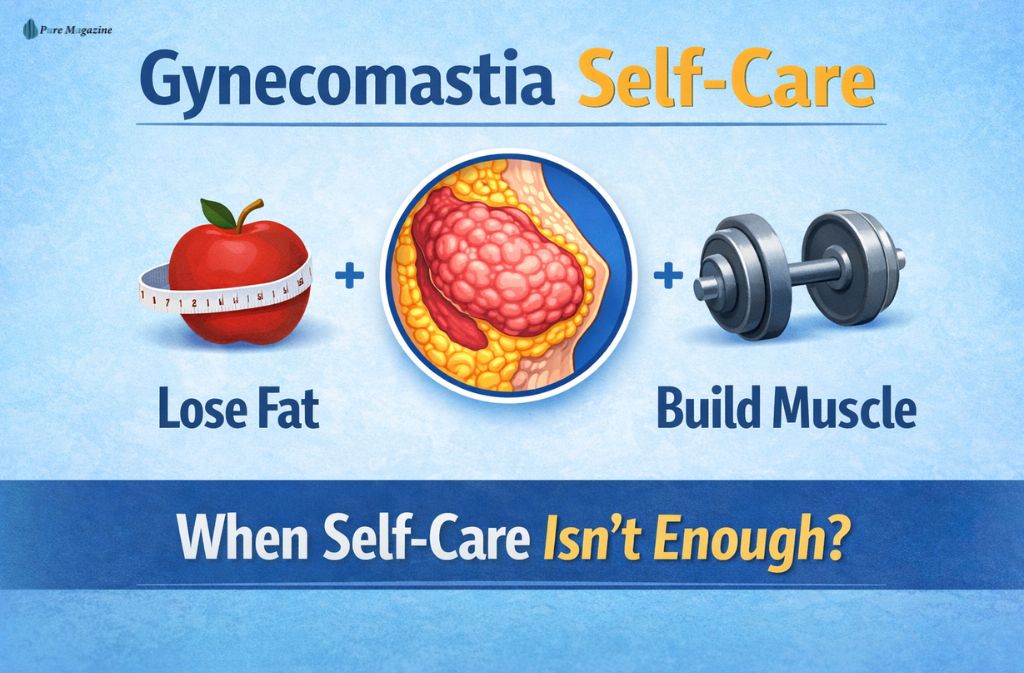
Gynecomastia affects millions of men worldwide, yet few topics create more confusion—or frustration. Chest enlargement in men isn’t just a cosmetic concern; it can influence posture, clothing choices, self-confidence, and everyday comfort. What makes it harder is the flood of conflicting advice online, ranging from extreme workouts to miracle supplements that promise results they can’t deliver.
Gynecomastia is the enlargement of male breast tissue caused by hormonal imbalance, excess fat, or a combination of both. Understanding that distinction is critical. Some forms respond well to lifestyle-based self-care, while others have biological limits that self-care alone cannot overcome.
This guide focuses on gynecomastia self-care that is evidence-aligned, realistic, and medically responsible as of 2025. You’ll learn what self-care can genuinely improve, how exercise and fat loss affect chest appearance, when progress typically plateaus, and how to recognize the point where professional input becomes the smartest next step.
What Gynecomastia Really Is (And Why Self-Care Outcomes Differ)
Gynecomastia is not a single condition. Results depend entirely on what type of tissue is causing the enlargement.
The Three Common Types of Gynecomastia
| Type | What’s happening | Can self-care help? |
|---|---|---|
| True gynecomastia | Excess glandular breast tissue | Limited |
| Pseudogynecomastia | Fat accumulation in the chest | Often yes |
| Mixed gynecomastia | Fat + glandular tissue | Partial |
Most adult men have mixed gynecomastia, which explains why lifestyle changes improve appearance without fully resolving the issue.
Key insight:
Gynecomastia self-care improves how the chest looks, not the underlying glandular structure.
Can Gynecomastia Be Treated With Self-Care?
Self-care can be effective—but only in the right context.
Self care works best when:
- Chest fullness is largely fat-related
- Overall, body fat is elevated
- Hormonal disruption is mild or lifestyle-driven
- The condition is recent
Self care has a limited impact when:
- Firm glandular tissue is established
- Gynecomastia began during puberty and persisted
- There is an ongoing hormonal imbalance
- Pain or tenderness is present
Understanding this early prevents unrealistic expectations and wasted effort.
The 2025 Gynecomastia Self-Care Framework
Step 1: At-Home Chest Assessment (Guidance, Not Diagnosis)
Observations that can help guide expectations:
- Firm, rubbery tissue beneath the nipple: glandular component
- Soft, diffuse fullness: fat-dominant
- Tenderness or sensitivity: active hormonal influence
Sudden growth, pain, nipple discharge, or one-sided enlargement should always be evaluated by a professional.
Step 2: Reduce Overall Body Fat (Highest-Impact Action)
Reducing body fat lowers estrogen production from fat tissue and improves chest appearance in fat-dominant and mixed cases.
Effective strategies:
- Moderate calorie deficit
- Resistance training 3–4 times per week
- Daily walking or low-intensity cardio
- Adequate protein intake
Ineffective approaches:
- Spot reduction
- Extreme crash dieting
- “Hormone detox” supplements
Even modest fat loss often produces visible chest changes.
Step 3: Strength Training for Chest Shape and Posture
Exercise does not remove glandular tissue, but it improves structure and definition.
Best movements:
- Bench presses and push-ups
- Incline dumbbell press
- Chest fly variations
- Dips (within shoulder-safe range)
Training the upper back and shoulders improves posture, reducing forward chest projection.
Step 4: Hormone-Supportive Lifestyle Adjustments
Lifestyle choices influence hormonal balance more than most people realize.
Helpful changes include:
- Limiting alcohol consumption
- Avoiding anabolic steroids and unregulated supplements
- Prioritizing consistent sleep
- Managing insulin resistance through balanced nutrition
These steps support stability and prevent progression.
Step 5: Mental Health Is Part of Self-Care
Gynecomastia frequently affects confidence and social comfort. Addressing this is not vanity—it’s well-being.
Practical strategies:
- Choose structured, well-fitted clothing
- Avoid constant body checking
- Track progress monthly rather than daily
- Seek professional support if anxiety or avoidance develops
Also Check: Maximize Your Wellness: Chiropractor Tips for Daily Living
What Gynecomastia Self-Care Cannot Do
Clarity here matters.
Gynecomastia self-care cannot:
- Remove established glandular breast tissue
- Reverse long-standing pubertal gynecomastia
- Replace the medical evaluation for concerning symptoms
In select early or hormonally active cases, clinicians may consider prescription hormone-modulating medications under medical supervision, but these are not self-care treatments and are only appropriate after proper evaluation.
When to See a Doctor About Gynecomastia
Self-care is valuable, but certain situations require professional input.
You should consider seeing a doctor if:
- Chest enlargement is painful or rapidly progressing
- One side is noticeably larger than the other
- No improvement occurs after 6–12 months of consistent self-care
- Gynecomastia developed alongside medication use
- Emotional distress is affecting daily life
Which Specialist Is Appropriate?
- Endocrinologist:
Best for evaluating hormonal imbalance, metabolic issues, or medication-related causes. - Board-Certified Plastic Surgeon:
Appropriate when gynecomastia is stable, long-standing, and structural. A consultation provides clarity on anatomy and options—it does not automatically mean surgery.
Early evaluation often prevents unnecessary delays and unrealistic expectations.
Also Read: Online Yoga Therapy Course: Healing Through Ancient Practice
Gynecomastia Self-Care vs Medical Options
| Approach | Fat reduction | Glandular tissue | Cost | Risk |
|---|---|---|---|---|
| Self-care | Yes | No | Low | Minimal |
| Medical therapy (early cases) | No | Partial | Medium | Moderate |
| Gynecomastia surgery | Yes | Yes | High | Surgical |
Common Gynecomastia Self-Care Mistakes
- Expecting exercises to remove glandular tissue
- Ignoring alcohol or medication effects
- Overtraining without fat loss
- Trusting supplement marketing
- Delaying evaluation despite worsening symptoms
Avoiding these mistakes improves outcomes.
FAQs:
Q. Can gynecomastia be treated naturally?
Natural approaches like weight loss, exercise, and lifestyle changes can improve fat-related chest enlargement (pseudogynecomastia). However, true gynecomastia caused by glandular breast tissue cannot be fully treated naturally and often requires medical evaluation.
Q. Will exercise get rid of man boobs?
Exercise can improve chest muscle tone, posture, and overall appearance, especially when excess fat is involved. It does not remove glandular breast tissue, so results depend on whether the chest enlargement is fat-based or glandular.
Q. How long should I try gynecomastia self-care before seeing a doctor?
Most men follow consistent gynecomastia self-care—fat loss, strength training, and lifestyle changes—for 6 to 12 months. If there is little improvement, worsening symptoms, or discomfort, a medical evaluation is recommended.
Q. Can gynecomastia be removed without surgery?
Fat-related chest fullness may be reduced without surgery through weight loss and exercise. Glandular gynecomastia usually cannot be removed without medical or surgical treatment, especially in long-standing cases.
Q. Does gynecomastia mean low testosterone?
Not necessarily. Gynecomastia is most often caused by an imbalance between estrogen and testosterone, not low testosterone alone. Many men with gynecomastia have normal testosterone levels.
Q. Is gynecomastia dangerous or a health risk?
Gynecomastia is usually benign and not dangerous. However, symptoms such as pain, rapid growth, nipple discharge, or one-sided enlargement should be evaluated to rule out other conditions.
Q. When should I see a doctor for gynecomastia?
You should see a doctor if gynecomastia is painful, worsening, asymmetrical, persistent despite self-care, or associated with medication use. An endocrinologist can assess hormonal causes, while a board-certified plastic surgeon can evaluate structural treatment options.
Conclusion
Gynecomastia self-care works best when expectations are realistic, and actions are consistent. Fat loss, strength training, and lifestyle improvements can meaningfully improve chest appearance and confidence—especially in fat-dominant and mixed cases. However, self-care has biological limits.
The most effective approach combines informed self-care with timely professional guidance. Clarity, not quick fixes, leads to the best outcomes.
Related: Longevity Complete: A Practical, Science-Led Approach to Daily Longevity Support