Ever typed “why disohozid are bad” into Google and thought, wait—what even is this? You’re not alone. That misspelling is surprisingly common. What you’re really looking for is Diazoxide (die-az-OX-ide). And honestly, yeah—the name sounds like something out of a chemistry exam, not a medication families have to deal with in real life.
But here’s the kicker: while the spelling is funny, the concerns about this drug are dead serious. Diazoxide isn’t your average “take two and call me in the morning” pill. It’s heavy-duty. It comes with real risks, and doctors don’t hand it out casually.
So let’s break it down—what diazoxide is, why it’s used, and why it can cause doctors, parents, and patients so much anxiety.
What Is Diazoxide, Really?
In plain English: diazoxide is a blood sugar–raising drug. Sold as Proglycem in the U.S., it’s used when blood sugar drops to dangerously low levels that don’t respond to food or glucose.
And here’s the twist: while most diabetes drugs are designed to lower blood sugar, diazoxide does the opposite. It blocks insulin release by holding potassium channels open in the pancreas. Less insulin = higher blood sugar.
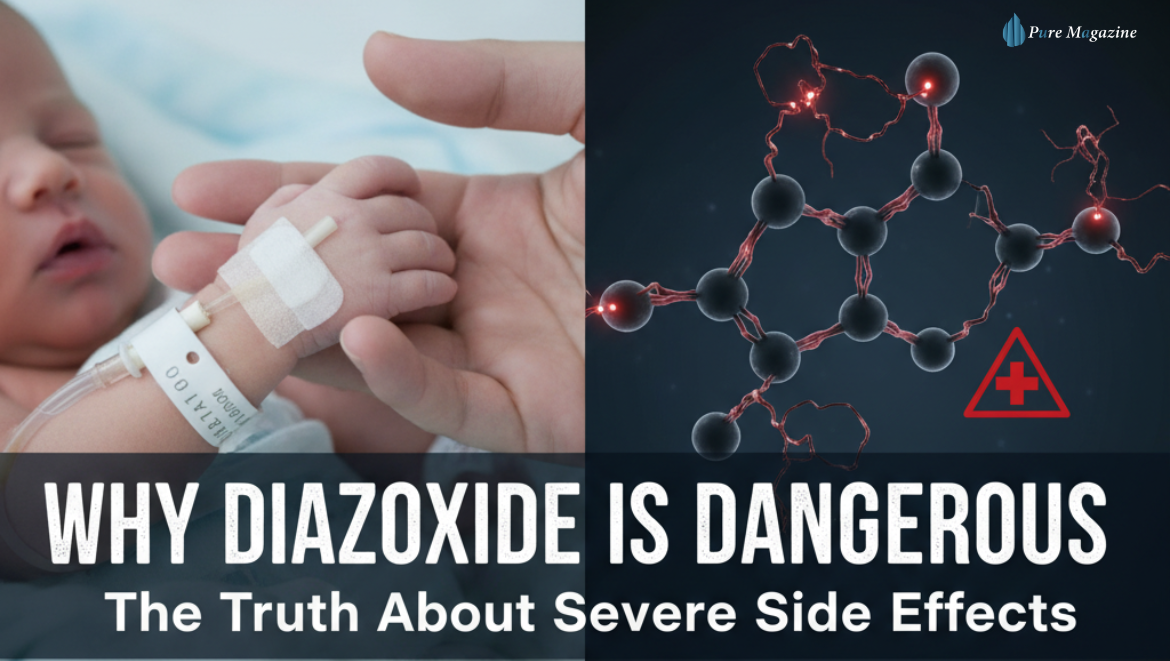
Sounds backwards, right? But for certain patients—especially infants born with congenital hyperinsulinism—it’s a lifesaver. These babies’ bodies churn out too much insulin, which can crash blood sugar to the point of brain damage.
A newer version called diazoxide choline exists, too. It’s extended-release, meant to smooth out dosing. But as you’ll see, it doesn’t erase the risks.
The Side Effects No One Likes Talking About
Here’s where things get dicey. Diazoxide isn’t considered “problematic” because of a few mild annoyances—it can cause some genuinely dangerous complications.
Fluid Retention: Not Just Swelling
We’re not talking about “my rings feel tight” kind of swelling. This drug makes the body hold onto sodium and water in a big way. Babies can blow up with fluid to the point where diuretics (water pills) have to be added just to keep things under control.
Pulmonary Hypertension: The One That Scares Doctors Most
In newborns, diazoxide has been linked to pulmonary hypertension—a condition where blood pressure inside the lungs shoots up. That can make breathing harder, or in the worst cases, lead to respiratory failure. Doctors treating fragile preemies know this risk all too well.
Blood Sugar Swings: Trading One Problem for Another
Ironically, the very drug meant to stop dangerous low blood sugar can sometimes push levels too high. Cue the glucose rollercoaster—hypoglycemia one moment, hyperglycemia the next. That’s why patients often need constant monitoring, sometimes even round-the-clock in the NICU.
Neutropenia: Immune System on Pause
Diazoxide can lower neutrophils, the white blood cells that fight off infection. Fewer neutrophils = higher risk of catching something nasty. This means extra blood tests and more watchfulness for fevers or illness.
Nerves and Heart: The Wild Cards
Some patients get headaches, dizziness, or rapid heartbeat. Rarely, doctors even pick up changes on heart scans. Again—this isn’t Tylenol.
Why Babies Are the Most Vulnerable
This is the hard truth: the tiniest patients are both the ones who need diazoxide the most and the ones who suffer the harshest side effects.
- On one hand, uncontrolled low blood sugar can cause seizures or lifelong brain damage.
- On the other hand: diazoxide can trigger lung and heart complications that newborns may not be strong enough to fight through.
That’s why NICUs use this drug under a microscope. Dosing has to be exact, side effects caught early, and backup support (like oxygen and ventilators) on hand if things go sideways.
For some babies, diazoxide is a bridge—they respond, stabilize, and eventually wean off. For others, it’s just a temporary stop before moving to surgery or alternative treatments. Genetics sometimes even predicts which kids will benefit and which won’t.
Drug Interactions: When Diazoxide Doesn’t Play Nice
If you’re on diazoxide (or your child is), your doctor wants to know every pill, supplement, or syrup in the cabinet. That’s because:
- Thiazide diuretics can worsen high blood sugar while being used to fight swelling.
- Blood pressure meds may mix unpredictably.
- Other diabetes drugs can throw glucose management into chaos.
- Liver-metabolized meds may not work as expected alongside diazoxide.
And if there’s pre-existing heart disease, lung issues, or pregnancy in the mix? The risks climb higher.
So… Why Use It At All?
With all this doom and gloom, you might be thinking: why not just ban the stuff?
Here’s why: for some patients, especially babies battling congenital hyperinsulinism, diazoxide is the only thing standing between them and permanent brain damage.
Doctors don’t pull it off the shelf casually. They weigh every risk, dose it cautiously, and watch like hawks. For some families, diazoxide buys precious time until the child grows stronger or surgery becomes possible.
FAQs
Q1. Why is diazoxide considered dangerous?
Diazoxide is considered risky because it can trigger fluid retention, lung problems, blood sugar swings, and immune suppression. These side effects can be severe, especially in infants.
Q2. Is diazoxide safe for newborns?
It can be life-saving for babies with congenital hyperinsulinism, but it’s not without risks. Newborns on diazoxide require NICU-level monitoring to prevent complications like pulmonary hypertension.
Q3. What are the most common side effects of diazoxide?
Common side effects include swelling (edema), high blood sugar, fast heartbeat, dizziness, and changes in blood counts. In infants, breathing problems are a major concern.
Q4. Are there alternatives to diazoxide treatment?
Yes. Alternatives may include octreotide injections, frequent glucose feeds, or, in severe cases, partial removal of the pancreas. The choice depends on the patient’s condition.
Q5. How do doctors monitor patients on diazoxide?
Doctors use frequent blood sugar checks, blood tests for immune cells, heart and lung scans, and weight monitoring to catch side effects early and adjust treatment safely.
Bottom Line
So, why is diazoxide considered problematic? Because it’s a drug with two faces:
- One side saves lives by preventing catastrophic hypoglycemia.
- The other side brings fluid retention, pulmonary hypertension, immune suppression, blood sugar swings, and cardiac concerns.
It’s not a “good” drug or a “bad” drug. It’s a tool—one that only works safely in the right hands, under constant medical supervision.
If you or your child is prescribed diazoxide, here’s the best advice:
- Ask every question, even the “obvious” ones.
- Stick to the monitoring plan.
- Don’t shrug off new symptoms.
- And remember—it’s spelled Diazoxide, not disohozid.
Because spelling quirks aside, this is one medication that demands respect.
Visit: Pure Magazine